So here we are, ready to unravel the mystery of borderline ECG. It's like diving into a treasure chest filled with secrets about your heart's electrical activity. Imagine this: your heart is like a finely tuned orchestra, and an electrocardiogram (ECG) is the conductor's baton, capturing every beat and rhythm. But what happens when the results aren’t crystal clear? That’s where borderline ECG comes into play. It’s a gray area, a zone where the results are not definitively normal or abnormal, leaving doctors and patients alike scratching their heads. Let’s dig deeper, shall we?
Now, before we get into the nitty-gritty, it’s important to understand why this matters. Borderline ECG isn’t just some random blip on the radar; it can be an early warning sign of potential heart issues. Think of it as your body’s way of saying, “Hey, pay attention!” In today’s fast-paced world, where heart health is often overlooked, understanding borderline ECG could be the difference between catching a problem early and letting it spiral out of control. So, let’s break it down step by step.
But wait, don’t freak out just yet. Having a borderline ECG doesn’t automatically mean you’re on the brink of a heart attack. It’s more like a yellow light on the highway, signaling caution. The key is to take it seriously, get the right follow-up tests, and work closely with your healthcare provider. So, buckle up, because we’re about to embark on a journey through the world of borderline ECG. Trust me, it’s going to be worth it.
Read also:How Old Is Sydney Sweeney Supposed To Be In The Handmaids Tale Discover The Truth Behind Her Role
Understanding the Basics of ECG
Before we dive headfirst into borderline ECG, let’s take a moment to understand what an ECG actually is. An electrocardiogram, or ECG (sometimes written as EKG), is a test that measures the electrical activity of your heart. It’s like a snapshot of your heart’s rhythm, showing how fast it beats, whether the rhythm is steady, and if there are any irregularities. It’s a non-invasive test, meaning no needles or fancy surgeries involved, just a few sticky pads placed on your skin.
Now, here’s the kicker: an ECG can detect a wide range of heart conditions, from arrhythmias to heart attacks. It’s like a detective tool for cardiologists, helping them piece together the puzzle of your heart health. But here’s the thing—sometimes the results aren’t black and white. That’s where borderline ECG steps in, leaving doctors scratching their heads and patients wondering what’s going on.
How Does an ECG Work?
Alright, so you’ve probably heard of an ECG, but how does it actually work? Well, it all starts with the heart’s natural electrical system. Every time your heart beats, tiny electrical signals travel through your heart muscle, telling it when to contract and relax. An ECG machine picks up these signals and translates them into a graph, showing the timing and strength of each electrical signal. It’s like reading a map of your heart’s activity, with peaks and dips representing different parts of the heartbeat.
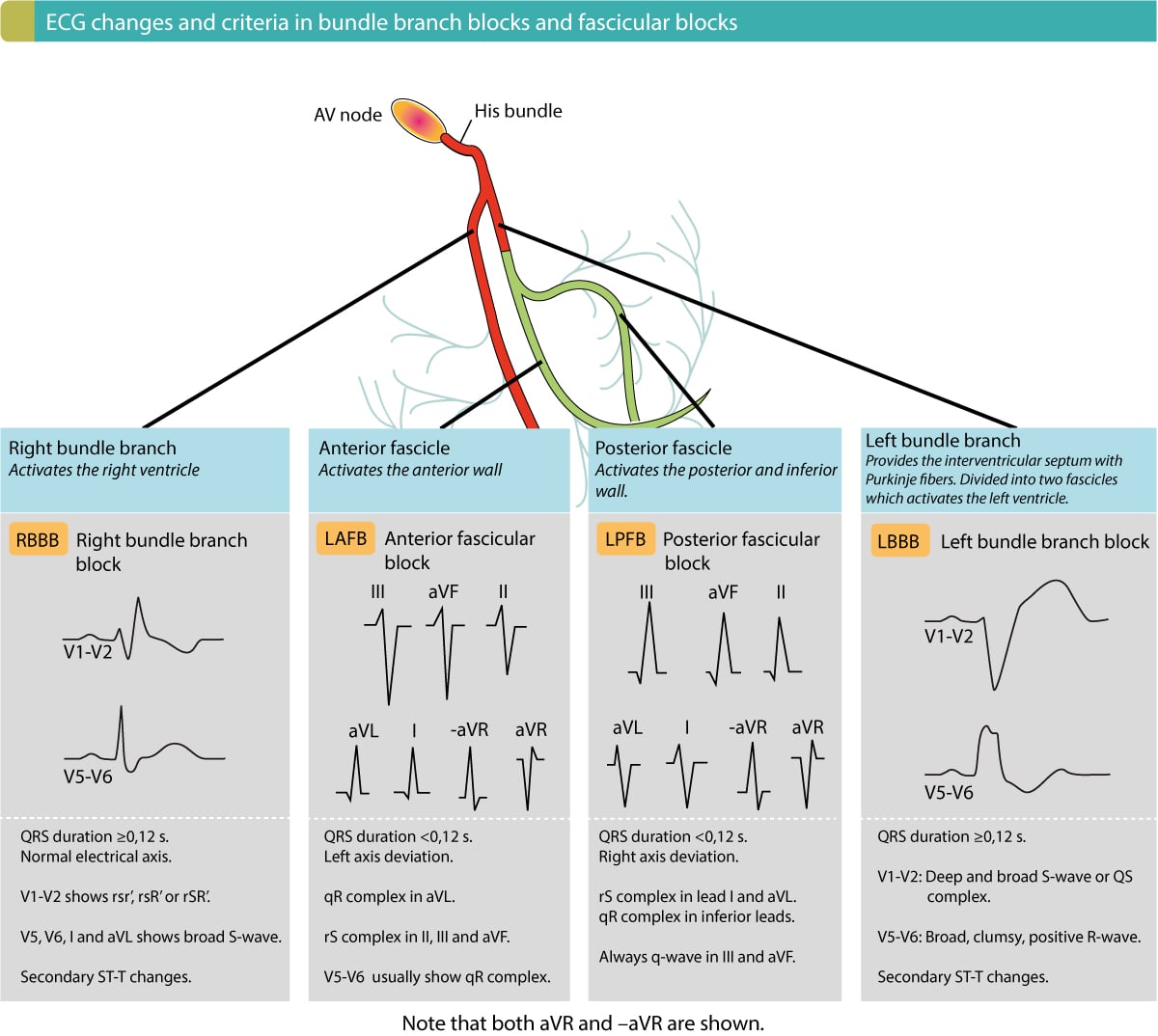
For instance, the P wave shows the electrical activity of the atria, the QRS complex represents the ventricles, and the T wave shows the heart’s recovery phase. If any of these waves look funky or out of place, it could indicate a problem. But here’s the tricky part: sometimes the waves are just a little off, not enough to scream “problem,” but enough to raise an eyebrow. That’s what we call a borderline ECG.
What Exactly is Borderline ECG?
Alright, so now that we’ve got the basics down, let’s zoom in on borderline ECG. Simply put, a borderline ECG is when the results of an ECG test fall into a gray area. It’s like being in limbo—your results aren’t clearly normal, but they’re also not clearly abnormal. It’s like walking the tightrope between two extremes, and it can leave both doctors and patients feeling a little unsure.
Think of it this way: imagine you’re taking a test, and your score is right on the cusp of passing or failing. You didn’t fail, but you’re not exactly flying high either. That’s what a borderline ECG feels like. The results might show slight deviations from the norm, but not enough to diagnose a specific condition. It’s a signal that something might be off, but it’s not definitive.
Read also:7th Street Burger Double Cheeseburger Calories A Guilty Pleasure You Need To Know
Common Features of Borderline ECG
So, what does a borderline ECG actually look like? Well, there are a few common features that doctors often see. For starters, you might notice slight changes in the intervals between waves, like the PR interval or QT interval. These intervals represent the time it takes for electrical signals to travel through different parts of the heart, and even small changes can be significant.
Another common feature is mild ST-segment changes. The ST segment is a part of the ECG that shows the period between ventricular contraction and relaxation. If it’s slightly elevated or depressed, it could indicate a problem, but not always. Sometimes, it’s just a quirk of your heart’s electrical system. Then there are T-wave abnormalities, which can show up as inverted or flattened T waves. Again, these changes might not mean much on their own, but they’re worth keeping an eye on.
Why Does Borderline ECG Matter?
Now, you might be wondering, why does borderline ECG matter so much? Well, here’s the thing: while a borderline ECG isn’t a definitive diagnosis, it can be an early warning sign of potential heart issues. Think of it as your body’s way of waving a red flag, saying, “Hey, something might be up here!” Ignoring it could mean missing out on catching a problem early, when it’s still treatable.
For instance, slight changes in the ST segment or T waves could be early signs of coronary artery disease, where the arteries supplying blood to your heart become narrowed or blocked. Or maybe it’s a hint of an arrhythmia, where your heart’s rhythm is a little off. Either way, catching these issues early can make a huge difference in your overall heart health.
Potential Risks and Red Flags
So, what are some red flags to watch out for with borderline ECG? Well, if you’re experiencing symptoms like chest pain, shortness of breath, or palpitations, it’s definitely worth investigating further. These symptoms, combined with a borderline ECG, could be signs of a more serious condition. But even if you’re feeling fine, a borderline ECG shouldn’t be ignored. It’s like ignoring a check engine light in your car—sure, everything might seem okay now, but it could lead to bigger problems down the road.
Another important thing to consider is your overall risk factors. If you have a family history of heart disease, high blood pressure, or high cholesterol, a borderline ECG might be more concerning. It’s like stacking the odds against you, and it’s worth taking seriously. Plus, if you’re a smoker, overweight, or lead a sedentary lifestyle, these factors can increase your risk even further.
How is Borderline ECG Diagnosed?
Alright, so how do doctors actually diagnose a borderline ECG? Well, it all starts with the ECG test itself. During the test, electrodes are placed on your chest, arms, and legs to measure your heart’s electrical activity. The results are then analyzed by a cardiologist or other healthcare professional, who looks for any deviations from the norm.
But here’s the thing: diagnosing a borderline ECG isn’t always straightforward. Sometimes, the results might be a little off, but not enough to diagnose a specific condition. That’s why doctors often look at the big picture, considering factors like your symptoms, medical history, and risk factors. They might also recommend additional tests, like an echocardiogram or stress test, to get a clearer picture of what’s going on.
Additional Tests to Consider
So, what are some additional tests that might be recommended if you have a borderline ECG? Well, one common test is an echocardiogram, which uses sound waves to create a picture of your heart. It can show how well your heart is pumping blood and if there are any structural abnormalities. Another test is a stress test, where your heart is monitored while you exercise on a treadmill or stationary bike. This can help detect issues that only show up during physical activity.
There’s also the Holter monitor, which is a portable device that records your heart’s activity over a period of time, usually 24 to 48 hours. It can catch irregularities that might not show up during a standard ECG. And let’s not forget blood tests, which can check for markers of heart damage or other conditions that might be affecting your heart health.
Treatment Options for Borderline ECG
Now, let’s talk about treatment options for borderline ECG. The good news is that, in many cases, treatment isn’t necessarily about fixing a specific problem. Instead, it’s about managing risk factors and keeping a close eye on your heart health. Think of it like maintaining a car—regular check-ups and tune-ups can keep things running smoothly.
One of the most important things you can do is make lifestyle changes. This might include eating a heart-healthy diet, exercising regularly, quitting smoking, and managing stress. These changes can make a huge difference in your overall heart health and might even help prevent more serious issues down the road.
Medications and Interventions
In some cases, medications might be recommended to help manage risk factors or treat underlying conditions. For instance, if you have high blood pressure or high cholesterol, medications like ACE inhibitors or statins might be prescribed. These can help lower your risk of heart disease and improve your overall health.
And let’s not forget about interventions like angioplasty or stent placement, which might be recommended if further testing shows signs of coronary artery disease. These procedures can help open up blocked arteries and improve blood flow to your heart. But again, these are usually reserved for more serious cases, and a borderline ECG alone typically isn’t enough to warrant such interventions.
Lifestyle Changes to Improve Heart Health
Alright, so we’ve talked about diagnosis and treatment, but let’s not forget the power of lifestyle changes. Making small tweaks to your daily routine can have a big impact on your heart health. For starters, try incorporating more fruits, vegetables, and whole grains into your diet. These foods are packed with nutrients that can help keep your heart in tip-top shape.
Exercise is another key player in the heart health game. Aim for at least 150 minutes of moderate aerobic activity or 75 minutes of vigorous activity each week. And don’t forget about strength training—building muscle can improve your metabolism and help keep your heart healthy. Plus, staying active can help you maintain a healthy weight, which is another important factor in heart health.
Stress Management Techniques
Now, let’s talk about stress. We all know it’s a part of life, but too much stress can take a toll on your heart. That’s why it’s important to find ways to manage it. Meditation, yoga, and deep breathing exercises can all help reduce stress and promote relaxation. And let’s not forget about good old-fashioned sleep—getting enough rest is crucial for heart health.
Another great way to manage stress is by staying connected with friends and family. Social support can be a powerful tool in maintaining mental and emotional well-being, which in turn can benefit your heart. So, don’t be afraid to lean on your loved ones when you need a little extra support.
Real-Life Stories: Living with Borderline ECG
Let’s take a moment to hear from real people who have dealt with borderline ECG. Sarah, a 45-year-old teacher, discovered she had a borderline ECG during a routine check-up. At first, she was worried, but after talking with her doctor and making some lifestyle changes, she’s feeling more confident about her heart health. “It was scary at first, but now I see it as a wake-up call,” she says. “I’m eating better, exercising more, and just taking better care of myself overall.”
Then there’s John, a 52-year-old engineer who was diagnosed with a borderline ECG after experiencing some mild chest discomfort. His doctor recommended further testing, which revealed some mild coronary artery disease. With medication and lifestyle changes, John’s condition has improved, and he’s feeling better than ever. “It’s all about being proactive,” he says. “Don’t wait until it’s too late to take care of your heart.”
Lessons Learned from Real-Life Experiences
So, what can we learn from these stories? First and foremost, a borderline ECG isn’t the end of the world. It’s an opportunity to take control of your heart health and make positive changes. Whether it’s through lifestyle modifications, medication, or additional testing, there are plenty of options available to help you stay healthy.
And let’s not forget the importance of regular check-ups and open communication with your healthcare provider. If you have concerns about your heart health, don’t hesitate to speak up. Your doctor